Redefining vision with the Galaxy spiral IOL:
A revolution in advanced technology optics
By: Prof. Claudette Abela-Formanek, Prof. Michael Amon, Prof. Gerd U. Auffarth, Mr. Allon Barsam, Dr. Başak Bostancı, Dr. Francesco Carones, Dr. Dean Corbett, Prof. Tiago Ferreira, Dr. Fernando Llovet, Mr. Sanjay Mantry, Dr. Alain Saad


What do patients expect from cataract surgery?
It is well established that a major patient expectation from cataract surgery is spectacle independence.1,2 However, patients typically do not just expect spectacle independence at distance, but also for near and intermediate activities, such as reading, working on their laptops, or indulging in hobbies.1–3
Trifocal IOLs, categorised as Full Range of Focus (FROF) lenses, were introduced 15 years ago and transformed cataract surgery outcomes with their ability to achieve spectacle independence at all distances.4–7 Despite this, trifocal IOLs do not guarantee patient satisfaction – their underlying diffractive optical principle can cause significant visual side effects, primarily glare and halos around light sources. Diffraction also leads to light loss (11-14% in trifocal IOLs),8 which negatively impacts contrast sensitivity.9 Photic phenomena and contrast sensitivity loss are worsened in dim-light conditions and can lead to difficulties in activities like nighttime driving or reading a menu.10,11 Thorough counselling is required to manage patient expectations, and only those who can tolerate some visual disturbances can be suitable candidates for diffractive trifocal IOLs.
In support of these compromises, Market Scope predicts global trifocal IOL growth to slow from +7.1% in 2025 to +3.5% in 2028,12 signalling the maturity of this diffractive lens category.
A recently published study confirmed the impact of dysphotopsia on patient satisfaction following cataract surgery.13 Patient-reported outcome measures (PROMs) were collected from over 2,500 patients across 26 countries via automated and anonymous email questionnaires using Rayner’s RayPRO digital PROMs platform. The study concluded that dysphotopsia was a stronger determinant of patient satisfaction than spectacle independence.
The increasing unwillingness of patients to compromise on their postoperative quality of vision has led to the growing popularity of IROF (Increased Range of Focus) lenses designed to improve upon the quality of vision limitations of trifocal IOLs. IROF lenses, such as the RayOne EMV, create an elongated focal point for an extended range of vision, whilst reducing visual disturbances by avoiding out-of-focus images and light splitting.14,15 Although good distance and intermediate vision can be achieved with IROF lenses, near visual acuity is reduced compared to diffractive FROF IOLs.16–18
It is clear that existing IROF and FROF lens options still require patients to compromise between quantity and quality of vision. As surgeons, we continue looking for the ideal presbyopia-correcting IOL that does not require patients to make any sacrifice: a FROF lens with minimal visual disturbances.
A ground-breaking approach:
The spiral IOL
At the 2024 ESCRS Congress, Rayner launched the world’s first spiral IOL – RayOne Galaxy. Developed in partnership with Prof. João Marcelo Lyra, a leading ophthalmologist from Brazil, the Galaxy IOL features a novel non-diffractive spiral optic designed with a proprietary artificial intelligence (AI) engine tuned for optimal patient outcomes.
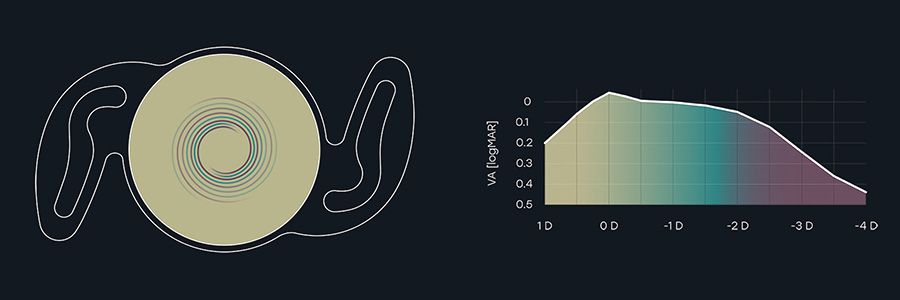
Instead of using diffractive elements or modulating spherical aberrations, the Galaxy IOL introduces a completely new mechanism of simultaneous vision: a continuous and progressive variance of power along the spiral tracks on the IOL optic, focusing light at every position along the defocus curve for a smooth and continuous full range of vision, from distance to near (Figure A).
Figure A. Schematic diagram of the Galaxy IOL (for illustrative purposes only).
Figure A. Schematic diagram of the Galaxy IOL (for illustrative purposes only).
The Galaxy IOL’s smooth, non-diffractive optic is crucial in minimising dysphotopsia. The absence of abrupt transitions or diffractive rings, in contrast to diffractive FROF lenses, decreases photic phenomena – particularly under low-light conditions. Additionally, the refractive spiral optic leads to 0% loss of transmitted light.
Like Rayner’s other hydrophilic RayOne lenses, the Galaxy IOL is made of their longstanding Rayacryl hydrophilic acrylic material. It also features the Amon-Apple 360° enhanced square edge for posterior capsule opacification prevention, plus Anti-Vaulting Haptic technology for intracapsular stability.
The Galaxy IOL is supplied fully preloaded in the same single-use injector system as the rest of the RayOne IOL family, and is available in toric powers for astigmatism correction – benefitting from the lens platform’s proven rotational stability and centration.19
Designed with AI – The future of IOL technology
The Galaxy IOL was engineered with the assistance of proprietary machine learning techniques to obtain the optimum IOL design needed to achieve a full range of vision, whilst minimising dysphotopsia. By systematically modelling millions of design iterations, the complex spiral optic was realised, and the development process of the new lens exponentially accelerated. Consequently, surgeons can offer their patients a lens technology that might not have otherwise been available for several years.
Putting the RayOne Galaxy IOL to the test
To determine whether the design advancements of the Galaxy IOL could translate into practical improvements in patient outcomes and satisfaction, a preclinical evaluation was conducted. 30 healthy subjects with no coexisting ocular pathologies were selected. The Real Artificial Lens Vision (RALV, DEZIMAL GmbH) device was used to simulate the visual experience following implantation of various IOLs, allowing participants to compare vision through three actual IOLs: a diffractive trifocal IOL, an enhanced monofocal IOL, and the spiral Galaxy IOL (Figure B). To ensure there was no natural accommodation of the eye during the simulations, cycloplegic drops were administered beforehand, with further effective pupil diameter size constriction to 3.55 mm by the RALV device.
Mean monocular visual acuity (VA) achieved by the Galaxy IOL for distance, intermediate and near was -0.05, 0.03, and 0.07 logMAR, respectively. Compared to the trifocal IOL, the Galaxy IOL achieved significantly better intermediate VA (p=0.005), while near and distance VA remained similar (p=0.315 and p=0.993, respectively). Importantly, distance vision with the Galaxy IOL was comparable to that of the enhanced monofocal IOL (p=0.14), while both intermediate and near VA were significantly improved (p≤0.001).
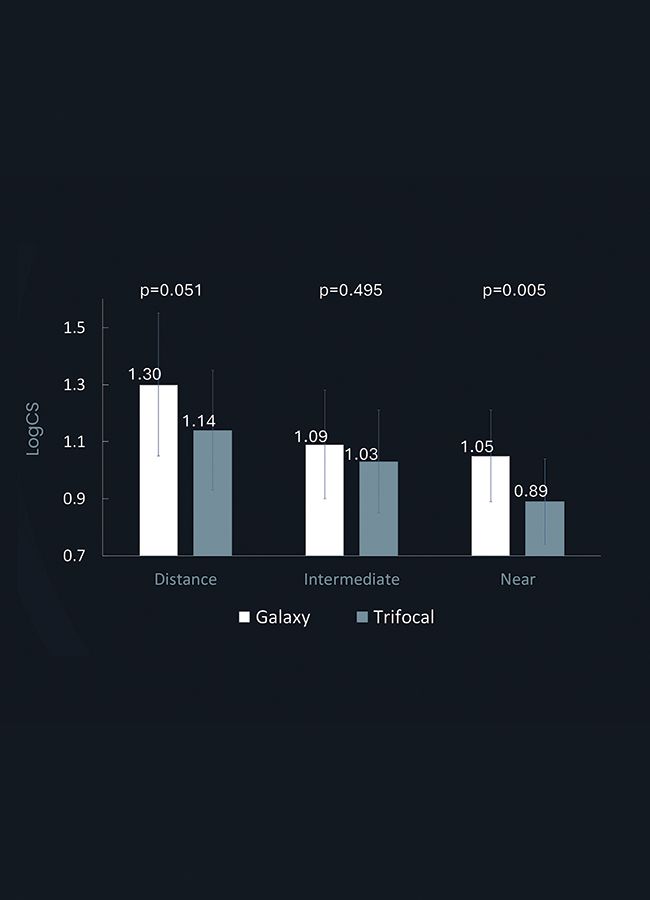
The Galaxy IOL defocus curve showed a full range of vision, with better VA at intermediate distances when compared to the trifocal IOL. Additionally, the Galaxy IOL demonstrated better contrast sensitivity (Figure C) than the diffractive trifocal IOL.
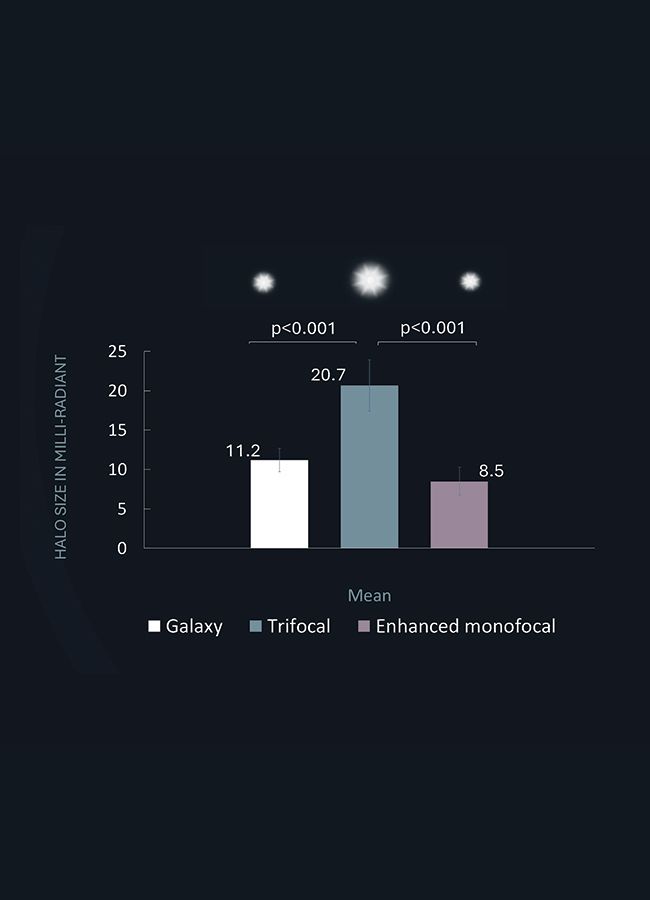
The Galaxy IOL halos were also significantly smaller than with the diffractive trifocal IOL (p<0.001), more closely resembling the size observed with the enhanced monofocal IOL (Figure D).
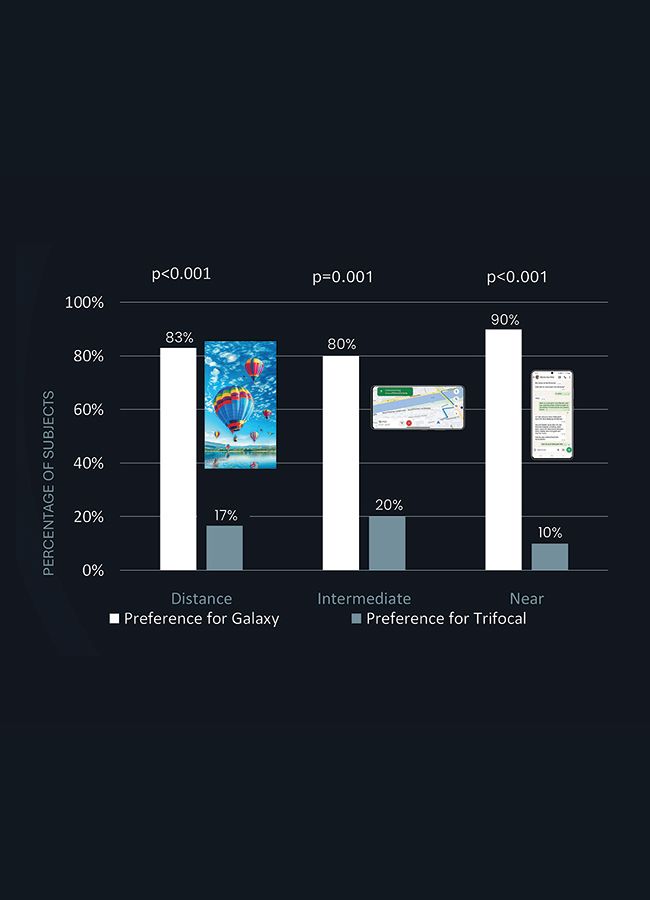
Lastly, a subjective lens preference test was performed, where subjects compared how text and/or image targets at various distances were visualised through the Galaxy IOL and the diffractive trifocal IOL. The majority of subjects preferred the Galaxy IOL at distance, intermediate, and near (p≤0.001) (Figure E), implying a natural and more comfortable optic to look through, compared with a diffractive trifocal IOL.
These preclinical findings suggested that the design innovations of the Galaxy IOL offers promising advantages in terms of visual acuity, contrast sensitivity, and patient satisfaction.
“Being able to compare real IOLs without implantation is hugely beneficial, and the results of the new Galaxy lens are quite astonishing.”
Prof. Michael Amon
Figure B. The Real Artificial Lens Vision (RALV) device setup.
Figure B. The Real Artificial Lens Vision (RALV) device setup.
Figure C. Contrast sensitivity.
Figure C. Contrast sensitivity.
Figure D. Halo size outcomes.
Figure D. Halo size outcomes.
Figure E. Subjective lens preference.
Figure E. Subjective lens preference.
Early clinical results from a multicentre data collection
An international collaborative project was started in July 2024, with 10 sites across Europe, Turkey and New Zealand participating in a post-market, real-world investigation to assess the clinical performance of the Galaxy IOL. All patients were eligible for premium presbyopia-correcting IOL implantation and underwent bilateral implantation with either RayOne Galaxy or RayOne Galaxy Toric. Postoperative follow-ups were conducted at 1 month and 3 months. The main outcomes assessed were VA, subjective refraction, defocus curve, and dysphotopsia.
“Galaxy sets a new milestone, providing very high spectacle independence with minimal quality of vision-related compromises.”
Dr. Francesco Carones
A total of 91 patients (182 eyes) were operated on, of which 57 patients were available for this analysis (57 patients at 1-month and 25 patients at 3-month follow-up). The study population had a balanced gender representation (43% males / 57% females). Mean age of the participants was 64 ± 9.5 years (range: 47 to 86 years). Patients with a range of refractive errors from hyperopia to low myopia were included. Toric and non-toric Galaxy IOLs were implanted in 52% and 48% of patients, respectively.
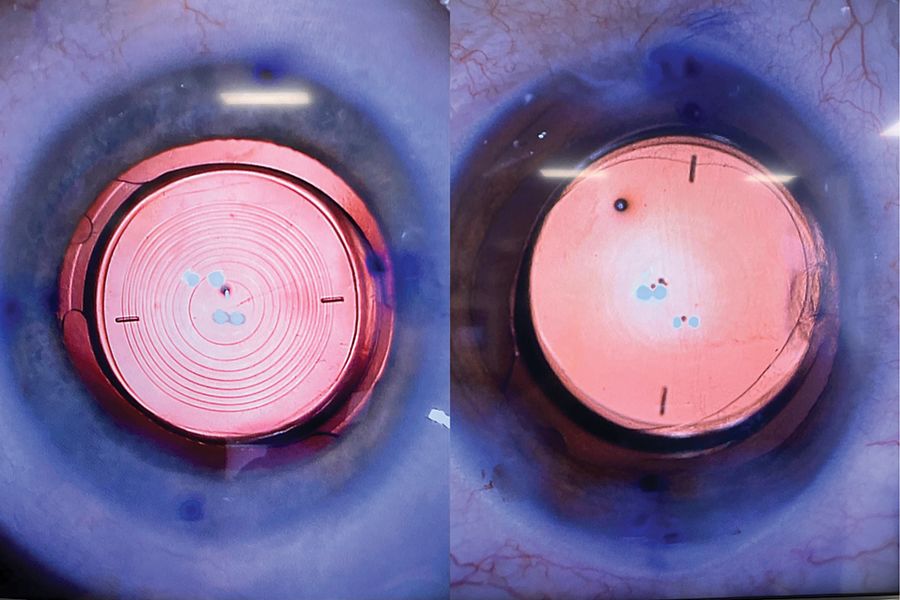
Intraoperative images taken during surgery (Figure F) showed a smooth optic surface free from the steps, discontinuities, or discrete annular zones associated with diffractive FROF IOLs. The Galaxy Toric IOL was observed to have good intraoperative stability, along with clearly visible alignment markings that enabled accurate IOL placement.
Figure F. Microscopic images of a diffractive trifocal toric IOL (left) and the Galaxy Toric IOL (right) – Courtesy of Mr. Allon Barsam.
Figure F. Microscopic images of a diffractive trifocal toric IOL (left) and the Galaxy Toric IOL (right) – Courtesy of Mr. Allon Barsam.
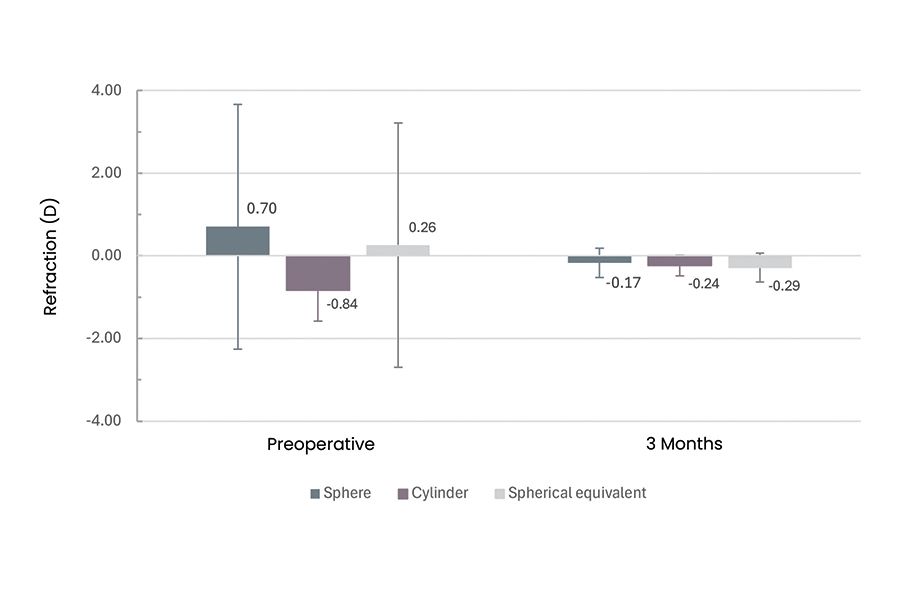
At 3 months, mean sphere, cylinder, and manifest refractive spherical equivalent (MRSE) were improved from 0.70 ± 2.96 D, -0.84 ± 0.74 D, and 0.26 ± 2.96 D preoperatively to -0.17 ± 0.36 D, -0.24 ± 0.25 D, and -0.29 ± 0.35 D, respectively (Figure G). Refractive outcomes showed good predictability: postoperative MRSE was within ±1.0 D of predicted refraction in 98% of eyes, within ±0.50 D in 78%, and within ±0.25 D in 52%.
Figure G. Subjective refraction.
Figure G. Subjective refraction.
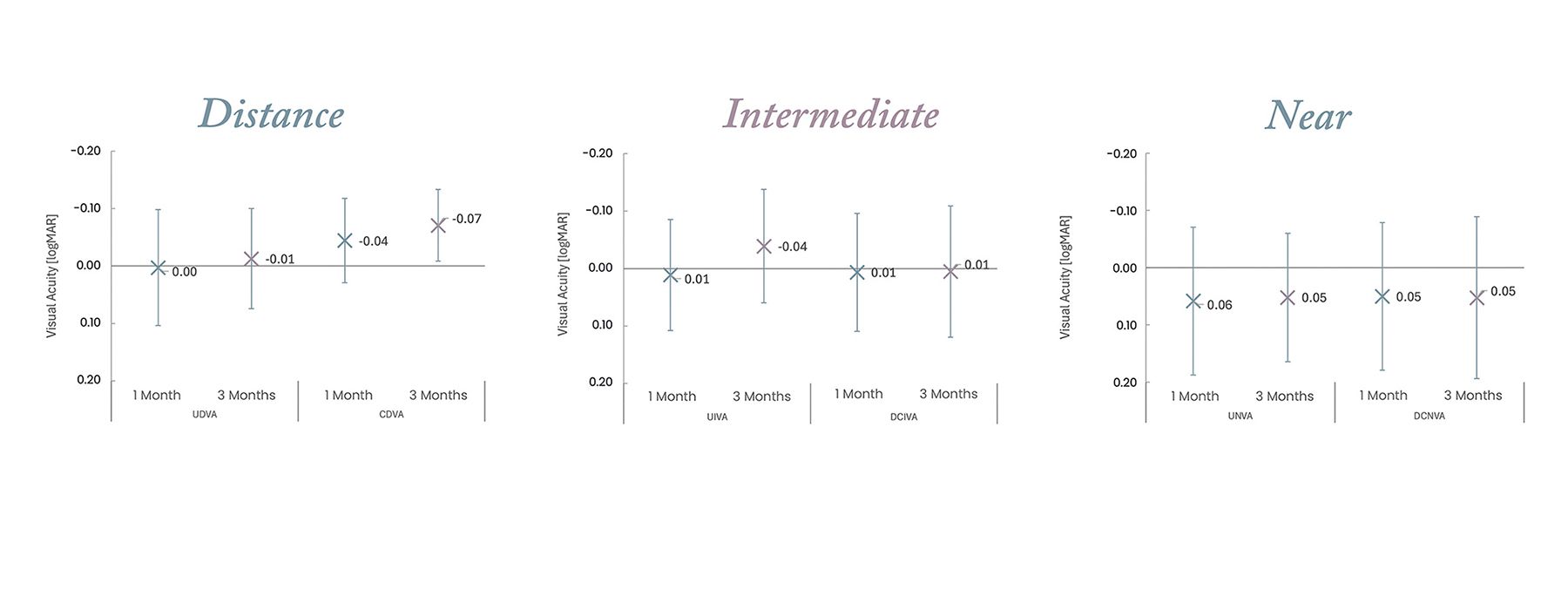
Binocular vision was excellent, with mean uncorrected and distance-corrected binocular VA better than 0.1 logMAR at all distances. VA was stable from 1 month onwards for all distances (Figure H).
Figure H. Binocular visual acuity outcomes.
Figure H. Binocular visual acuity outcomes.
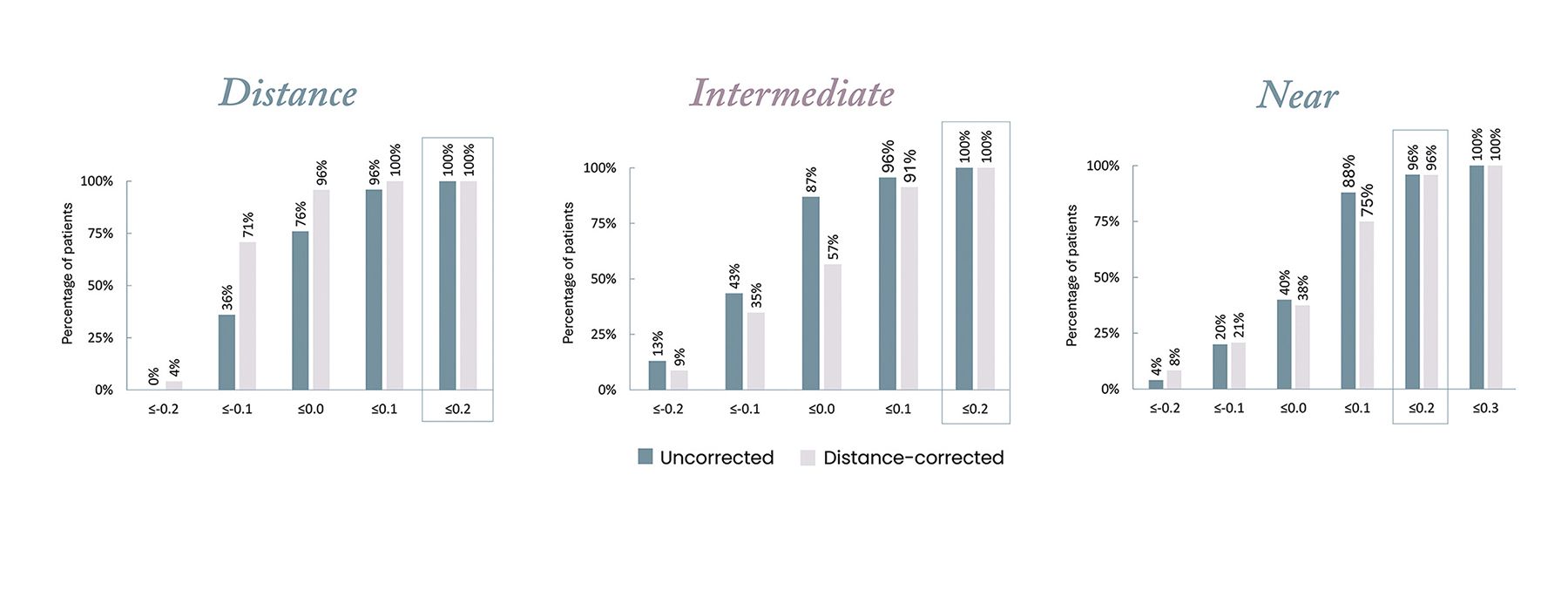
At 3 months, functional uncorrected VA of 0.2 logMAR or better was achieved in 100% patients for distance and intermediate vision and in 96% patients for near vision. Uncorrected VA of 0.1 logMAR or better was achieved in 96% of patients for distance and intermediate vision and in 88% patients for near vision (Figure I).
Figure I. Binocular visual acuity at 3 months – Cumulative outcomes.
Figure I. Binocular visual acuity at 3 months – Cumulative outcomes.
Monocular and binocular defocus curves showed stable defocus patterns at 1-month and 3-month follow-ups. The binocular defocus curve showed a full range of vision extension up to -2.8 D, equating to 36 cm, and VA of 0.2 LogMAR or better across a ~4 D range (Figure J). The smooth and elongated defocus contrasts with the peaks and dips commonly seen with diffractive trifocal IOLs.17,20
Figure J. Monocular and binocular defocus curves of the Galaxy IOL.
Figure J. Monocular and binocular defocus curves of the Galaxy IOL.
“One day after surgery my first patient was reporting no halos – this is extraordinary for a FROF IOL.”
Prof. Gerd U. Auffarth
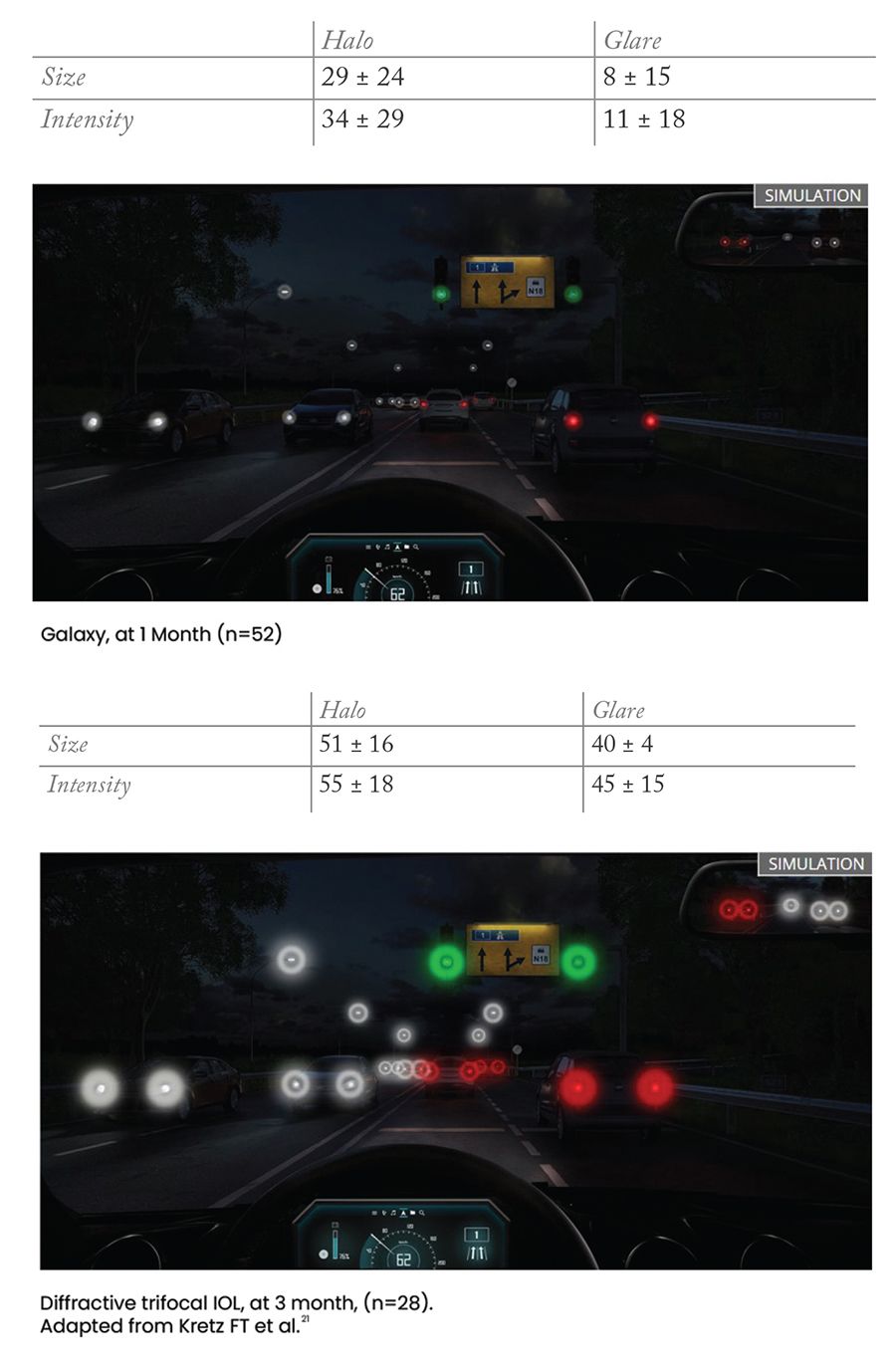
On dysphotopsia testing using a halo and glare vision simulator, mean halo and glare size and intensity scores at 1 month follow-up were substantially lower than that reported for state-of-the-art diffractive trifocal IOL models,21,22 and visual quality was noticeably better preserved (Figure K).
Figure K. Halo and glare simulator results for the Galaxy IOL (top) and a diffractive trifocal IOL (bottom).
Figure K. Halo and glare simulator results for the Galaxy IOL (top) and a diffractive trifocal IOL (bottom).
“With my patients not reporting any bothersome dysphotopsia, I can’t see a reason to now use a trifocal IOL – I don’t have to compromise.”
Mr. Allon Barsam
What do these results mean for cataract and presbyopia patients?
While the final analysis of the complete Galaxy IOL study cohort is forthcoming, initial results from this interim analysis paint a very promising picture, and are consistent with the findings of the preclinical evaluation.
Simply put, the Galaxy IOL is a FROF IOL with a minimally dysphotopic profile, providing the best of both worlds with spectacle independence and high optical quality over a full range of vision for maximal patient satisfaction. This represents a leap forward in IOL capabilities and the outcomes that surgeons can offer to their patients.
“My patients could not be more satisfied – with excellent vision at all distances, and no dysphotopsia.”
Dr. Fernando Llovet
By comprehensively addressing the most significant patient requirements in a single platform, the Galaxy IOL has the potential to cater to a broader population of patients than existing IOL technologies. As quality of vision is preserved, the Galaxy IOL can be more forgiving in patients with high visual demands, providing spectacle independence for all their daily needs, including nighttime driving, and allowing them to maintain an active lifestyle and continue their hobbies following cataract surgery.
Conventional wisdom in cataract surgery until now was that quantity and quality of vision shared an inverse relationship due to the immutable optical properties of diffractive FROF IOLs. The impressive performance of the Galaxy IOL in both preclinical and clinical evaluations shows that it is possible to achieve excellent spectacle-independent vision at all distances while providing high-quality vision free from bothersome photic disturbances. With the creation of the world’s first spiral IOL, patients may no longer have to compromise between quantity and quality of vision, marking the first step towards a new paradigm of more natural vision with less compromise.
For references, please download the PDF supplement